50 Shades of Plantar Fasciitis (Ultimate Guide)
Your feet are marvellous. Each one has 26 bones, 33 joints, and more than 100 muscles. Needless to say, the design by Mother Nature is complicated but perfect. Every part is crucial as it is.
That is why when this single element of the structure - Plantar fascia - fails, you feel excruciating pain growing gradually or breaking out at once. 150+ websites I've browsed through offer ambiguous cures, and 100+ scientific articles I've read eagerly investigate the pain millions of people struggle with daily.
We spent 381 hours to get to the core for you to reach the long-awaited relief you crave.
Do I have plantar fasciitis?
To know if you have PF you should at first examine yourself carefully and answer following questions.
- Does my foot hurt most at the bottom of the arch next to the heel? Is my arch sore?
- When I touch the hurt area, do I feel sharp and stabbing pain? Is it a bit red, warm and swollen at times?
- Is the pain hitting worst in the morning with the first steps, and wearing out with further activity?
- Does it come back towards the end of the day, and increase with the time spent weight-bearing?
- When running, does it hurt more when I am pushing off rather than landing?
- Does it hurt terribly whenever I walk barefoot?
- Do I feel tightness in the Achilles tendon and calves?
- Has my gait and posture changed lately?
- Have I changed my exercising pattern? Do I spend most time of the day on my feet?
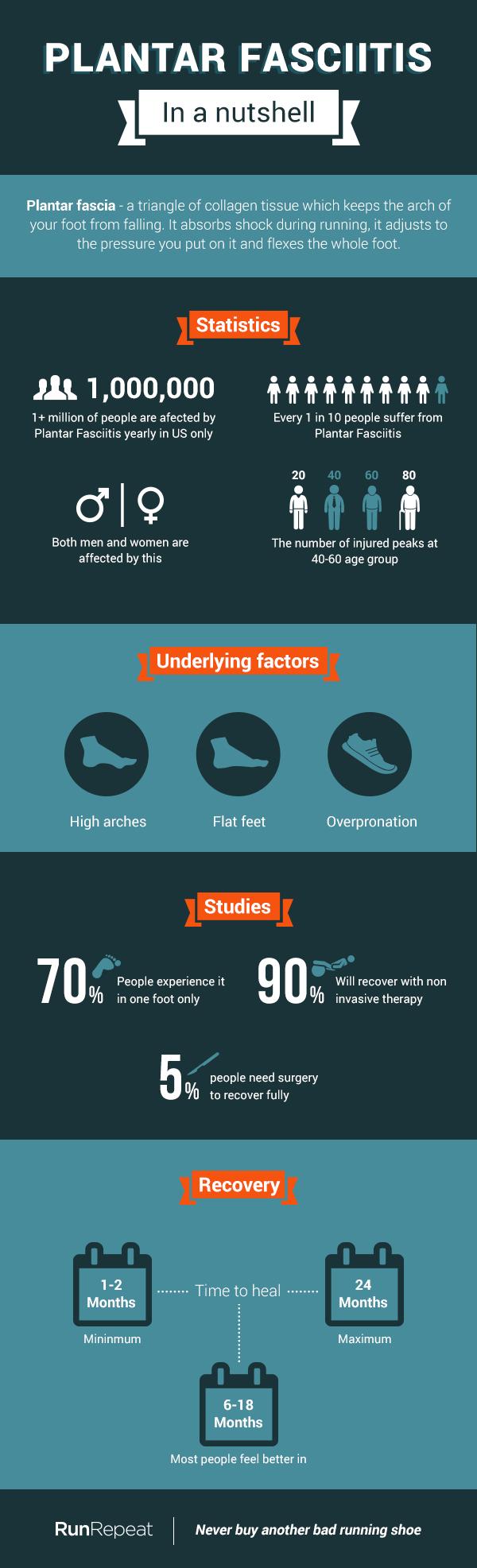
If everything above is a yes, you're in a good company. According to this string of studies, Plantar fasciitis (PF) is the most common cause of rearfoot pain in runners.
What exactly is Plantar Fasciitis?

And now you must be thinking: that's my problem, so how do we deal with it?
Not so fast! There are several conditions that can be easily mistaken with PF, and it is worthy to first make sure you are addressing THE issue, right?
Doctor Stephen L. BARRETT et al, these qualified specialists at Practical Neurology and much more assert that in some cases what feels somewhat like PF is:
- Achilles Tendinopathy (pain worsens with exercise, particularly when you start and finish)
- Tarsal tunnel syndrome (it hurts more in the upper part of the foot, pain is burning and doesn't stop at night)
- Policeman's heel (pain under the heel bone, similar to bruise, without radiating to the arch)
- Calcaneal stress fracture (it hurts at the back of your heel, increasing with activity)
- Heel spurs (although you may have heel spurs, which look like tiny spurs on the heel bone on MRI, they have nothing to do with PF;
- Plantar Fascial Rupture (you cannot stand on your toes, there's a bruise on your arch and when you palpate it, it hurts severely near the heel. It also makes you limp)
Among other causes of heel and arch pain there are Calcaneal Apophysitis (mostly affects boys of 6-10 y.o) and Systemic Disorders (have to be properly diagnosed with additional medical tests).
Your feet are your ultimate support, and ignoring the symptoms of PF can result in chronic pain that will interfere with your routines and may lead to pain in the knees, hips or back because of how it affects the way you walk, says medical research.
I am a Runner. Am I at risk of having Plantar Fasciitis?

Avoiding running isn't the panacea, though. Research shows that plantar fasciitis is regular among the common folk just as much. Basically, any overuse or extra tension put to fascia can initiate micro-tearing that might circle into the chronic pain.
According to the research done by this group of scientists, those are the main risk factors for PF in non-athletes.
- Reduced ankle mobility
- Engaging in a new sport or fitness activity
- Gaining weight
- Pregnancy (in the last 10 weeks)
- Work-related weight-bearing
- Wearing worn, poorly constructed, inadequately supporting shoes
- Ageing
- Diabetes and arthritis
- Hormonal abnormality (and other metabolic disorders)
- Excessive driving (PF in the right foot), etc.
You are in the risk group, you feel like your case is Plantar Fasciitis, for sure. What's next?
First of all, consider going to a physician or a podiatrist. He or she will definitely be able to help you with managing pain and facilitate the healing.
Let's take a closer look at what to expect at the doctor's office.
Don't be surprised if the doctor takes a look not only at your feet but your whole "kinetic chain", i.e every body part that moves when you're running: spine, pelvis, hips, knees, ankles and toes.
You may be also checked for muscular tonus and neurovascular response, and asked to move around a bit and describe your pain. What for?
- Gait and posture: pain in the injured limb makes you limp and may be reflected in the way you walk.
- Neuro-response: pain in the heel may as well be a result of a Systemic Disease or nerve infringement.
- Muscles of the leg: stiff calves and reduced ankle movement are usually aligning PF.
- Back of your foot: Achilles tendon thickening can both mean PF and Achilles tendinopathy, depending on the degree of tenderness.
- Feet: sensitivity to touch at the place where the plantar fascia attaches to the heel is a clear indicator of Plantar Fasciitis, radial pain in the arch is also very common.
- Toes: stiffness in the big toe can develop alongside with plantar fasciitis or calf muscle injuries.
Research suggests that there are also a few alarming symptoms that may clearly point at different serious issues:
- Nerve damage in feet and legs: numbness or a tingling sensation in your foot.
- Bone infection: your foot feels hot and you have a high temperature of 38°C (100.4°F) or above.
- Arthritis: your heel is stiff and swollen.
With the absence of these or any other additional symptoms usually, no further tests are necessary. However, your physician can consider directing you to undergo:
- Specific blood tests to rule out inflammation, hormonal disorders, diabetes, etc.
- Ultrasound (useful in ruling out soft tissue pathology of the heel)
- Imaging (used to confirm unclear cases of plantar fasciitis or to rule out other heel pathology)
- MRI (more expensive procedure that clearly shows the thickening of fascia, indicating the stage of PF).

How to heal Plantar Fasciitis
Based on studies and reviews we can assume that depending on how developed PF is, varying treatment can be chosen. Some studies suggest that 2 broad stages can be singled out:
Stage 1. Reactive/ early disrepair (the fascia responds by thickening and stiffening as the reaction to excess stress).
According to this study, it is more likely to develop after a sudden increase of tension put on feet. If caught at this stage, it yields a prognosis of a faster recovery.
Treatment: managing pain, reducing the load on damaged tissues, stretching the compensating muscles and tendons.
1. Non-steroidal anti-inflammatory drugs (NSAIDs): such as aspirin or ibuprofen. Those are on the menu since Day 1, designed to put the pain down. NSAIDs are commonly used to treat plantar fasciitis, but fail to resolve the pain in 20% of people, according to Dr. LA Molloy's study.
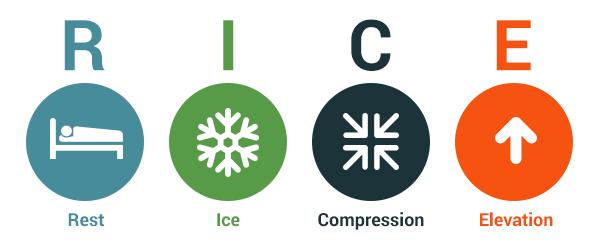
2. RICE therapy: deciphered as Resting, Icing, Compressing, Elevating. This approach helps to manage pain and reduce inflammation.
- Reduce activity first and keep it t low levels for a month at least, avoid walking barefoot, especially when you make first steps out of bed.
- Ice the place of injury, using a plastic bag wrapped in a towel. Do it 2 or 3 times a day and hold it for 5 to 10 minutes, with the breaks of 30 min at least. Repeat to put the pain and inflammation down.
- Compress the foot by wrapping it in an elastic bandage or using athletic tape. It decreases inflammatory processes and prevents the arch from further injury when you move. Research suggests that in the short term, low-Dye taping significantly reduces the pain associated with plantar fasciitis.
- Elevate your foot above the level of your heart to minimise swelling, whenever you rest.
3. Pain-relieving stretches.
If you kept exercising, experienced dull to stabbing pain, ignored the growing discomfort, delayed visiting the doctor or if you fall under more than 2 risk factors simultaneously, chances are that you moved to Stage 2 of PF.
Stage 2. Degenerative/ later disrepair (chronical damage and a constant load of fascia result in collagen degeneration within the tissue).
It is reversible, though the recovery is prolonged, and can be from as short as 1 month up to 24 months.
Treatment: a variety of mechanical, medical and physiotherapeutic cures are available. Special attention should be put to facilitating the load on a damaged tissue to strengthen it and prevent further reoccurrence.
Be not afraid: we are taking a close look at most popular and most effective ways to heal Plantar Fasciitis, as to current state of scientific research.
Conservative treatment
First thing first: let's manage the symptoms. If you choose from supportive devices, they are as following:
 Athletic tape: Taping can take the burden of supporting off your arch, so it is recommended to use the low dye tape technique or any kinesiology tape. This study from 2005 shows that taping significantly reduces the pain associated with plantar fasciitis in short-term.
Athletic tape: Taping can take the burden of supporting off your arch, so it is recommended to use the low dye tape technique or any kinesiology tape. This study from 2005 shows that taping significantly reduces the pain associated with plantar fasciitis in short-term.
 Gel heel cups: Wearing extra heel cushion will reduce the shock put to the place where fascia attaches to the heel bone. The best way to choose an over-the-counter pair of cups is to place one in your shoes and try walking - you should feel some immediate relief.
Gel heel cups: Wearing extra heel cushion will reduce the shock put to the place where fascia attaches to the heel bone. The best way to choose an over-the-counter pair of cups is to place one in your shoes and try walking - you should feel some immediate relief.
 Night splint: a splint is a device that looks like a rough boot, designed to keep your foot and Achilles tendon in stretched position. It works because it doesn't allow the fascia to compress at night and form scar tissue, which otherwise hurts when you make first steps in the morning.
Night splint: a splint is a device that looks like a rough boot, designed to keep your foot and Achilles tendon in stretched position. It works because it doesn't allow the fascia to compress at night and form scar tissue, which otherwise hurts when you make first steps in the morning.
The downside is discomfort, as you literally disturb the natural position of rest of your foot. Many studies confirm that night splints are very effective even in the cases of prolonged chronic pain but are intolerable with some patients. Night splints are recommended to be used for 1-3 months and should be considered as an intervention before an invasive treatment, as clearly outlined in this study.
 Walking cast: this daylight brother of night splint looks much like a ski boot and is mostly prescribed when a person has a full or partial Plantar Fascia rupture. However, some studies suggest wearing this mechanical supportive for several weeks as a final conservative step. In one study a short-leg cast worn for a minimum of three weeks was found to be an effective form of treatment for chronic plantar heel pain.
Walking cast: this daylight brother of night splint looks much like a ski boot and is mostly prescribed when a person has a full or partial Plantar Fascia rupture. However, some studies suggest wearing this mechanical supportive for several weeks as a final conservative step. In one study a short-leg cast worn for a minimum of three weeks was found to be an effective form of treatment for chronic plantar heel pain.
 Orthotics: It is proven that these mechanical attributes are designed to lift your arch properly and lessen the amount of tension so that no further damage is done. Trials confirm the effectiveness of foot orthotics in patients with plantar fasciitis, and it was found that prefabricated and custom foot orthotics can decrease rear foot pain and improve foot function.
Orthotics: It is proven that these mechanical attributes are designed to lift your arch properly and lessen the amount of tension so that no further damage is done. Trials confirm the effectiveness of foot orthotics in patients with plantar fasciitis, and it was found that prefabricated and custom foot orthotics can decrease rear foot pain and improve foot function.
The difference between aforementioned corrective devices and Shoe inserts is in their construction. While the former has a deep heel cup, hard base, and a cushioned sweet spot, the latter are spongy or rubber footbeds. As shown in this comparative study, various shoe inserts can indeed provide some relief. Orthotics, in their turn, reduce the overwork of the fascia allowing it to heal.
 Massage: although ice massage and direct massage of the fascia bring pleasure, the scientific evidence of its effectiveness is anecdotal. However, deep tissue massage of calves with a focus on muscle trigger points appears to aid in the healing of the fascia and provides significant pain decrease, according to a study by Saban B et al.
Massage: although ice massage and direct massage of the fascia bring pleasure, the scientific evidence of its effectiveness is anecdotal. However, deep tissue massage of calves with a focus on muscle trigger points appears to aid in the healing of the fascia and provides significant pain decrease, according to a study by Saban B et al.
This sci research, and this national study by medical doctors confirm that most patients will get better via conservative treatment alone. In other words, using several of these devices plus doing stretches and exercises can give your feet necessary support to heal on their own, as it was mentioned in some papers.
Medical cures for Plantar Fasciitis
If the pain persists for 3 or 6 months your physician is likely to offer you some medical procedures to take care of your pain. A further step is invasive ways to treat chronic conditions. Sounds scary to me.
Let's face the fear of the unknown: there are non-invasive and invasive cures. And there also are experimental options. Shall we take a closer look?

Injections:
- Corticosteroid: a powerful anti-inflammatory, by far the most popular with runners. This particular research by Gohiya A et al demonstrates 70% success rate in easing symptoms in 1 month, but not in 6 months.
Though it is proven to give immediate relief, in a long-term perspective steroid injections do more harm than good. These studies show that cortisol shots slow down the healing and may induce plantar rupture in 10% of the patients. It is recommended not to give more than 3 steroid injections within a year.
- Platelet-rich plasma (PRP): a relatively new injection type. In short, it is a shot of the plasma collected from you, which is rich with platelets and thus able to release growth factors to stimulate healing in degenerative tissue, as established in a study by Sampson S et al. You should consider this variant if conservative therapy failed, say the authors of this article.
PRP is safe to use, and in many cases is more effective and durable that Cortisone injections, asserts this research. Many studies were done to compare plasma and corticosteroid shots, and the findings confirm that PRP has a potential to reduce pain and may be preferable to its counterpart. Take a closer look at the study in International Orthopaedics, Foot & Ankle International and Foot (Edinburgh, Scotland) for more details.
- Botulinum toxin A (BTX-A): a much-investigated injection, that is referred to as very effective in the scientific literature. In this trial, a significant reduction of pain during weight-bearing to about 50% was seen 6 weeks after injection. Some other studies prove the efficacy of Botox injections and point out its durability as contrasted to corticosteroid injections. See more from Foot&Ankle International.
Among other injections, your clinician can offer you Lidocaine (a medication used to numb tissue), Hyperosmolar dextrose (a sugar solution intended to reduce pain level), or Autologous/ Whole blood (your own blood for decreasing pain and inflammation) shots. There is little to no evidence to confirm the long-lasting effect of these types of invasive interventions.
There's more to it:
 Acupuncture: this procedure can be really challenging for first-timers, but some studies claim that standard and electroacupuncture works well in treating patients with chronic heel pain; especially with the addition of trigger point acupuncture in poor or non-responders.
Acupuncture: this procedure can be really challenging for first-timers, but some studies claim that standard and electroacupuncture works well in treating patients with chronic heel pain; especially with the addition of trigger point acupuncture in poor or non-responders.
 Dry needling is also used for symptom relief. A needle is inserted into the myofascial trigger point in the heel and manipulated in various directions. Controlled trials show a significant reduction in heel pain in patients after 4 weeks of therapy.
Dry needling is also used for symptom relief. A needle is inserted into the myofascial trigger point in the heel and manipulated in various directions. Controlled trials show a significant reduction in heel pain in patients after 4 weeks of therapy.
 Extracorporeal shockwave therapy is a non-invasive treatment in which a device is used to pass acoustic shockwaves through the skin to the affected area. The shockwaves are generated using electrohydraulic, electromagnetic or piezoelectric energy. It can be either a series of sessions or a single procedure. The footnote of the procedure is stimulating the healing of the fascia, as asserted by the studies.
Extracorporeal shockwave therapy is a non-invasive treatment in which a device is used to pass acoustic shockwaves through the skin to the affected area. The shockwaves are generated using electrohydraulic, electromagnetic or piezoelectric energy. It can be either a series of sessions or a single procedure. The footnote of the procedure is stimulating the healing of the fascia, as asserted by the studies.
The downside of this treatment is possible pain during the procedure. Plenty of research has been made, but the success rates differ considerably, as can be seen from this research review by British Institute for Health and Clinical Excellence.
Negligible side-effects that reduce the necessity for a surgical procedure certainly make this therapy the next step after non-effective conservative treatment, as agreed by researchers from Journal of Orthopaedic Surgery and Research, Arch Orthopaedic and Trama Surgery and Journal of Bone and Joint Surgery.
Interestingly enough, one study comparing ESWT with conventional treatments even found out that there was no difference in efficacy of both, 3 months after the end of therapy.
Still, the research is ongoing, as no treatment has proven to have a good enough success rate without substantial side-effects. Experimental treatments include Low-level laser therapy, Cryotherapy, Marrow stimulation techniques, Cryopreserved human amniotic membrane, etc.
What is the worst case scenario for PF?
 About 5 % of people still need surgery after unsuccessful conservative treatment. You can take one of 2 roads here: have a surgery on the fascia itself or on the corresponding calf.
About 5 % of people still need surgery after unsuccessful conservative treatment. You can take one of 2 roads here: have a surgery on the fascia itself or on the corresponding calf.
Plantar fasciectomy: this is by far most popular cardinal way to treat PF. A surgeon removes part of the plantar fascia from the heel bone, thus battling the cause for irritation. It can be done openly or endoscopically. The latter has less possible complications, as only 2 small incisions are made. Other complications may include arch flattening, nerve injury, calcaneal fracture, and long recovery time.
Most patients are satisfied with the operation results, as successful healing has been confirmed at short-, mid- and long-term follow-up, as to this research by Patrick Wheeler et al. Surprisingly, athletic people seem to have a better post-op state, says a trial in Foot Ankle Int.
 Sometimes this surgery may be accompanied with removing a heel spur or stretching or loosening specific foot nerves. Heel spurs - small bony elements that can grow on the feet bones - do not cause PF, though they may appear alongside it. It is advised to remove them only if they produce discomfort and irritate soft tissues.
Sometimes this surgery may be accompanied with removing a heel spur or stretching or loosening specific foot nerves. Heel spurs - small bony elements that can grow on the feet bones - do not cause PF, though they may appear alongside it. It is advised to remove them only if they produce discomfort and irritate soft tissues.
Gastrocnemius recession: a more ambiguous procedure aiming at releasing the calf tightness. While it is stated that tense calves have a direct impact at fascia strain, surgical lengthening of the gastrocnemius can be a viable option, say J. Maskill, D. Bohay, and J. Anderson.
One study derived out of 126 cases shows that in combination with successful recovery exercising scheme this surgery yields very good results with low morbidity rate.
Cryosurgery: yet newer procedure, that involves inserting small cryoprobe to destroy pathologic tissue at -70 C temperature. Research shows an impressive 77% success rate. It is still in the experimental stage, but so far the results seem promising, as per the article in Foot Ankle Surg Journal.
What we are sure about is that every case of PF has its unique characteristics, and only after a consult with a qualified physician or podiatrist, the treatment can be established.
Scientific evidence states: painkillers in any form is not a solution to PF. It has to be treated, preferably in the early reactive stage. Do it by giving your feet rest, supporting the arch, strengthening and stretching the feet AND calf muscles and tendons.
If in late disrepair stage the crucial point is the correct combination. Based on the sources we've reviewed the order can be as follows:
- Manage the pain. Keep track of medication - there is always a limited time to use it.
- Always remember to RICE your feet. Since Day 1 until symptoms go away.
- Start putting the load on fascia slow. Stretch every day, starting BEFORE you make the first step.
- Pick your supportive device - the arch needs to be placed right and rested for at least 4 weeks.
- If symptoms persist for more than 6 months, consider injections, acupuncture or ESWT.
- If your physician recommends you a surgery after 12 months of chronic fascial pain - consider it.
The first 3 points are a must-do, regardless of how long you have been struggling with PF. If you keep to those and show no additional symptomatic, your feet shall heal, as to the scientific word.
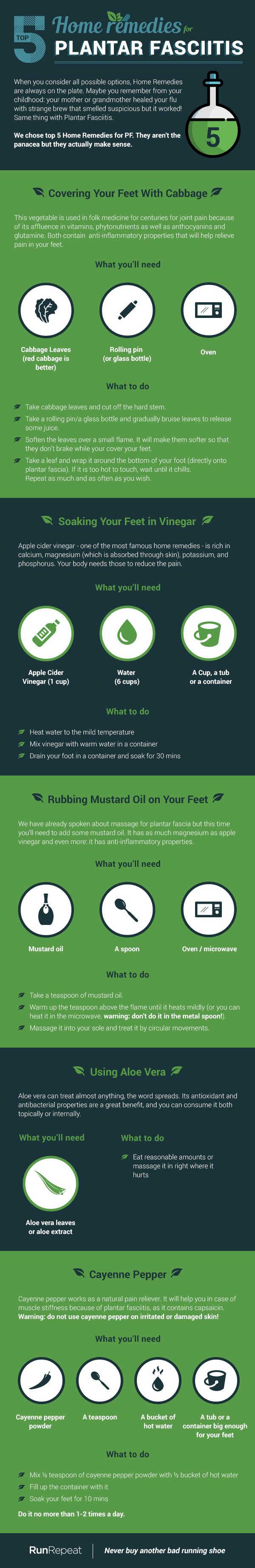
Enough with medical cures. Now discover how to treat Plantar Fasciitis at home.
How to stretch and exercise with PF?
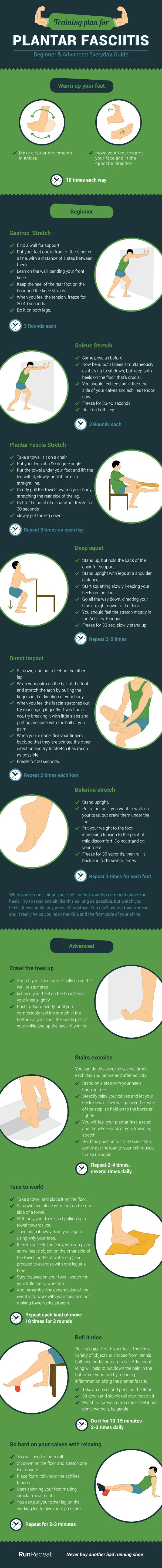
If you are face-to-face with Plantar Fasciitis, let me introduce you to your new everyday ritual: stretching and special exercising. While stretching is mostly directed at releasing the tension in muscles and tendons, exercising aims at teaching your feet endurance. In other words, you have to show your arches how much load you want to put on them.
Learning takes time, and in a while, you will be able to strengthen your arches with more intense and impactful activity.
We have created a pattern of most becoming exercises that are effective according to the scientific articles we've processed.
Now when you're equipped with things to do to heal your plantar fasciitis, we can take a look at what can help us rocket the process. There is absolutely no way to heal PF in the degenerative stage in under 1 month, but there are some boosters you can use to prevent the outbreaks.
How to prevent Plantar Fasciitis and Speed up Treatment
- Move
- Run on soft surfaces, and increase the load on your feet wisely. Stop running for 2-4 weeks at least when having PF.
- Do not walk barefoot first thing in the morning, unless you warmed up your feet in the bed. When having PF keep supportive footwear on, at all times.
- Switch between high and low impact exercising patterns. When having PF, try swimming or bicycling instead of running, introduce it slowly back only when pain diminishes.
- Eat
- Add the right oil. Focus on getting more Omega-3 Fatty Acid: it has potent anti-inflammatory agents.Try eating coldwater fish like halibut, mackerel, salmon, and herring. Switch to Olive oil in salads: it has oleocanthal, which works in much the same way as NSAIDs.
- Spice it up! Go for curcumin or ginger. Both of them reduce levels of inflammation markers. Curcumin, also known as turmeric, can be consumed in capsules. Fresh or powdered ginger goes well in hot drinks and teas.
- Get painkiller fruit. Pineapple is full of bromelain, which is considered to relieve pain. Citrus fruit got flavonoids that can lessen inflammation. Berries have anthocyanins, which have strong antioxidant and painkilling properties.
Footnote: none of move-and-eat advice work alone. You need to both exercise to show your body that you need that inflammation to strengthen your arch and pass and treat it with the right diet, which means less refined sugars and processed foods and more fresh and leafy nutrients.
Nature has its way of helping us to soften injuries, and many of supporting symptoms can be addressed by a variety of weird analogue home treatments.
The outcomes
Running out of PF is not an easy task. You need to examine your symptoms carefully, evaluate your physical state and look out for belonging to the risk groups.
After getting a consult from a certified podiatrist and confirming the injury, you need to adapt new habits of stretching and exercising, which, as was shown, can facilitate healing on its own.
Pick your supportive devices and begin conservative rehabilitation. If you are one of those 1 in 10 people, who see no positive changes in 6 months - consider going at it aggressively, with ESWT or injections. Surgery helps at most 7 in 10 people, so be sure to have kept to diet and guided physical activity before you decide.
You will recover from Plantar Fasciitis, as many thousands of people get better every month. The science states: your body has immense potential of healing PF. Tissue inflammation is its means of learning your will, and it is absolutely oriented at recovery. Keep in mind that pain is a symptom and you need to heal the core.
Make sure you treat your feet smart, and you will never stumble upon PF again. Period.